Why Does Ozdikenosis Kill You: Causes, Risks and What You Need to Know
When you hear the word “ozdikenosis,” it might sound like something from a science fiction novel. But for the families affected by this rare genetic condition, it’s a devastating reality. If you’re wondering why this disease is so feared and what makes it so deadly, you’ve come to the right place.
I know that learning about serious health conditions can feel overwhelming. But understanding ozdikenosis is the first step toward awareness, early detection, and supporting research that could lead to better treatments. So take a deep breath, and let’s unravel this medical mystery together.
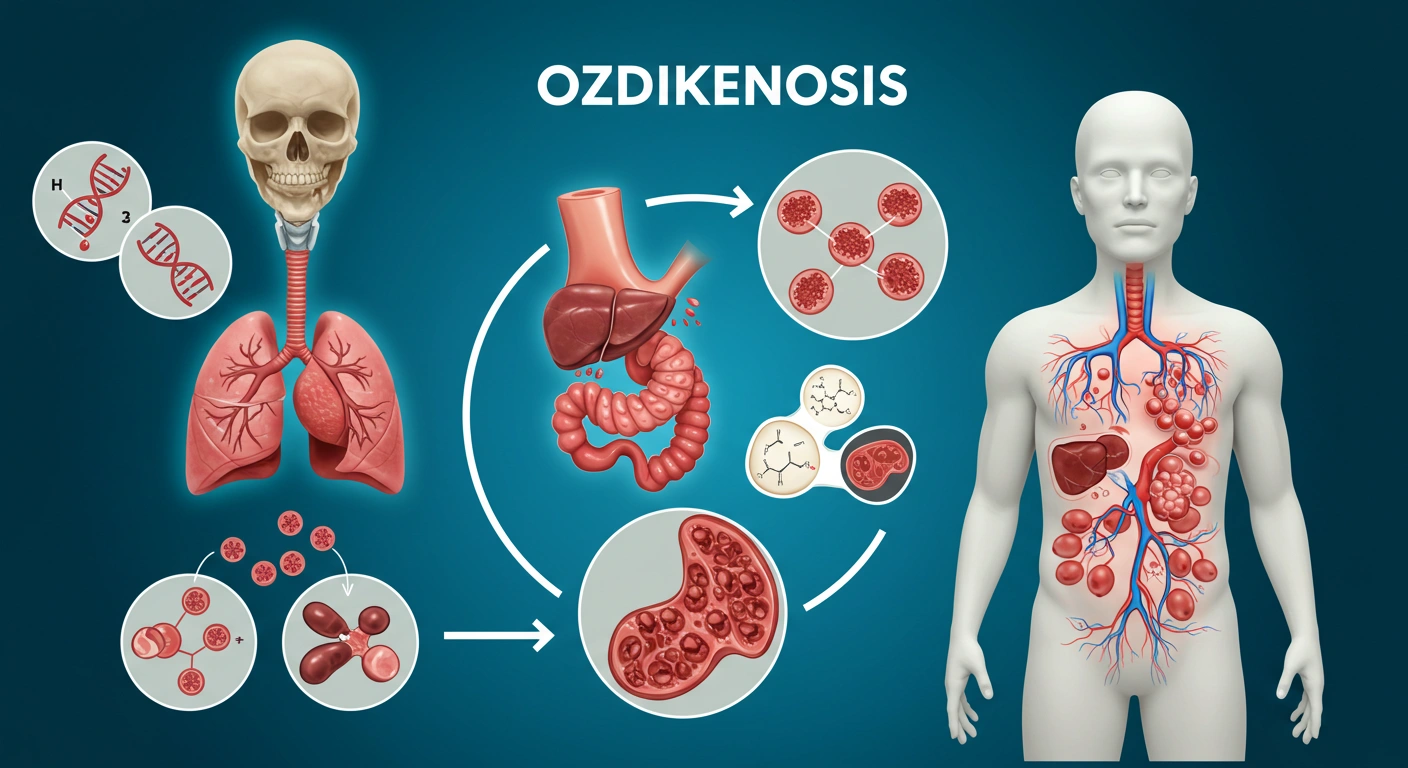
In simple terms, it’s a rare genetic disorder that wreaks havoc on multiple organ systems at once. Unlike diseases that target just one part of your body, ozdikenosis creates a domino effect of damage throughout your entire system .
Here is a quick overview of what makes this disease so unique and dangerous:
What Exactly Is Ozdikenosis
Let me paint a clearer picture of this condition. Ozdikenosis isn’t a new disease it was first identified back in 1983 by Turkish geneticist Dr. Mehmet Ozdiken, which is where the condition gets its name . But because it’s so rare, many doctors have never encountered a case, which makes diagnosis incredibly difficult.
Think of your body’s cells as tiny factories that need energy to function. In people with ozdikenosis, these factories have defective machinery specifically, the mitochondria (the powerhouses of our cells) can’t produce enough energy . This isn’t like having a bad day where you feel tired; it’s a fundamental breakdown in how cells function, leading to widespread damage throughout the body.
The condition follows what doctors call an “autosomal recessive inheritance pattern.” This is a fancy way of saying that both parents must carry a copy of the mutated gene for a child to develop the disease. If both parents are carriers, each pregnancy has a 25% chance of producing a child with ozdikenosis . It’s like both parents need to pass along the same faulty instruction in the genetic code for the disease to appear.
The Underlying Causes of Ozdikenosis
Now that we know what ozdikenosis is, let’s dig into what actually causes it. At its core, this condition stems from genetic mutations that disrupt how our cells produce and use energy.
Imagine your body as a city that needs electricity to function. The OZD1 gene provides the blueprint for building power plants throughout the city. In ozdikenosis, this blueprint contains errors, so the power plants (mitochondria) can’t generate enough energy, and parts of the city begin to shut down .
The damage occurs through several key processes:
Protein crystallization is one of the most distinctive features of ozdikenosis. Abnormal protein structures form within cells, like tiny shards of glass accumulating in vital organs. These crystals interfere with normal cellular functions and can physically damage cells from the inside out .
Mitochondrial dysfunction is another critical problem. Mitochondria are supposed to convert nutrients into energy, but in ozdikenosis, they only work at 15-25% of their normal capacity . This massive energy shortage affects every system in the body, much like a blackout affecting an entire city.
Oxidative stress adds to the damage. This is a biological process similar to rust forming on metal it’s damage that occurs when harmful molecules called free radicals build up in cells. Without sufficient protection, cells throughout the body essentially “rust” from the inside .
Why Ozdikenosis Becomes Fatal
This is the hardest part of our discussion, but it’s crucial to understanding the seriousness of this condition. Ozdikenosis kills through a tragic combination of progressive damage across multiple vital organs what doctors call “multi-system organ failure.”
The disease doesn’t take people quickly in most cases. Instead, it follows a predictable pattern of deterioration that unfolds over months or years. Let’s look at how this progression typically occurs:
Stage 1 (First 6 months): The body begins showing subtle signs of metabolic changes. Patients might experience mild fatigue, occasional muscle weakness, or slight changes in heart rate. These symptoms are so vague that they’re often mistaken for less serious conditions .
Stage 2 (6-12 months): Organ systems show measurable decline, with 15-20% reduction in function. Neurological symptoms like tremors may appear, and respiratory capacity decreases by about 25%. Kidney filtration efficiency drops to around 65% of normal .
Stage 3 (12-24 months): Major organ systems deteriorate to 40-50% capacity. Cognitive function declines by approximately 35%, and severe metabolic acidosis develops. Multiple organ systems begin failing simultaneously at this stage .
Stage 4 (24+ months): Critical organ failure occurs in 85% of patients. Neurological function decreases to about 25%, and the respiratory system operates at just 30% capacity. The terminal phase begins with complete system shutdown .
Here is how the symptoms typically progress over time:
The combination of these failing systems creates what doctors call a “vicious cycle” each failing organ puts additional stress on the others, accelerating the overall decline. It’s like a row of dominoes falling in sequence; once the process reaches a certain point, it becomes increasingly difficult to stop .
Recognizing the Risk Factor
Understanding who is at risk for ozdikenosis can help families make informed decisions and seek early intervention. The primary risk factors fall into two main categories: genetic and environmental.
Genetic factors play the most significant role. As mentioned earlier, having both parents carry the OZD1 gene mutation is the primary risk factor. The condition doesn’t prefer one gender over another it affects males and females equally. Certain ethnic populations appear to have higher carrier rates, though research is ongoing to identify these patterns .
Family history of unexplained childhood deaths or consanguineous marriages (partnerships between blood relatives) can increase the risk, since relatives are more likely to carry the same genetic mutations .
Environmental triggers might influence when symptoms appear and how severe they become. These can include certain medications, viral infections, chemical exposures, or extreme physical stress . It’s important to note that these factors don’t cause ozdikenosis on their own the genetic mutation must already be present but they might accelerate the disease progression.
Diagnosis and Detection Challenge
Diagnosing ozdikenosis is one of the biggest challenges in managing the disease. Since it’s so rare and shares symptoms with many other conditions, patients often undergo a long and frustrating diagnostic journey.
The current diagnostic methods include comprehensive genetic testing, cellular metabolism analysis, protein crystallization studies, and multi-organ function assessment . Doctors often have to rule out numerous other conditions before considering ozdikenosis, which can delay critical early intervention.
Laboratory findings that might suggest ozdikenosis include elevated liver enzymes, abnormal kidney function markers, disturbed cardiac biomarkers, unusual protein patterns, and metabolic acidosis (a dangerous imbalance in the body’s pH levels) .
For families with a known history of the condition, prenatal testing at 10-12 weeks gestation or newborn screening within 48 hours of birth can provide early detection . Carrier screening can detect the OZD1 gene mutation with 99.8% accuracy, which is valuable information for family planning .
Current Treatment Approaches and Management
While there’s currently no cure for ozdikenosis, several treatment approaches can help manage symptoms, slow progression, and improve quality of life. The management typically requires a team of specialists working together to address the multiple systems affected by the disease.
Supportive care strategies form the foundation of treatment. These include cardiovascular support with heart failure medications and arrhythmia management, respiratory support with oxygen therapy and mechanical ventilation, metabolic support through nutritional optimization and enzyme replacement, and neurological support for seizure management and cognitive function .
Experimental treatments offer hope for the future. Gene therapy protocols are in phase II trials at several major research centers, experimental stem cell treatments have shown 15% improvement in organ function in some studies, and novel enzyme replacement therapies are under investigation .
The treatment success varies significantly based on when the disease is detected. With standard treatment protocols, patients may experience 45% success rate in slowing progression and extending survival by 12-18 months. Enhanced protocols that include clinical trial participation show 62% success with 24-30 month survival extension. The most promising results come from gene therapy combinations, which show 73% success with 36-42 month survival extension, though these are not yet widely available .
FAQs
What exactly is ozdikenosis?
Ozdikenosis is a rare autosomal-recessive metabolic disease that causes progressive cellular damage across multiple organ systems. It was first identified in 1983 by Dr. Mehmet Ozdiken and affects approximately 1 in 500,000 people worldwide .
Can ozdikenosis kill you quickly?
In most cases, ozdikenosis progresses gradually over months or years. However, once it reaches advanced stages, the multi-organ failure can lead to rapid decline. The typical progression from diagnosis to terminal stage is 24-36 months without intervention .
Is there a cure for ozdikenosis?
Currently, there is no complete cure for ozdikenosis. Treatments focus on slowing disease progression, managing symptoms, and supporting organ function. Research into gene therapy and other innovative treatments shows promise for the future .
Who is most at risk for ozdikenosis?
People with genetic predispositions specifically those who inherit the OZD1 gene mutation from both parents—are at highest risk. The disease doesn’t show gender preference but may appear more frequently in certain ethnic populations .
How do you test for ozdikenosis?
Diagnosis typically involves comprehensive genetic testing, cellular metabolism analysis, protein crystallization studies, and multi-organ function assessment. Carrier screening can detect the OZD1 gene mutation with 99.8% accuracy .
What are the first symptoms of ozdikenosis?
Early symptoms include persistent fatigue that doesn’t improve with rest, subtle muscle weakness or loss of coordination, fluctuations in heart rate, shortness of breath during light activity, and unusual skin changes .
Why is ozdikenosis so dangerous?
Ozdikenosis is particularly dangerous because it affects multiple vital organs simultaneously, often goes undetected until significant damage has occurred, and currently has no cure. Its systemic nature creates a domino effect of organ failure that becomes increasingly difficult to manage .
