Dry Socket Vs. Normal Socket After Tooth Extraction
There’s no joy in getting a tooth pulled, but what you eat after is crucial to both your healing and how you’ll feel as the days go by. Knowing how to tell the difference between a healing socket and a dry socket will prepare you to know what is normal and when it is time to ask for help.
What Happens After a Tooth Extraction
When your dentist pulls a tooth, it leaves behind a hole in your jawbone known as a socket. Your body instinctively responds, quickly mobilizing to protect that exposed area.
Once removed the socket starts to fill with blood almost immediately. Platelets adhere to one another and a protein known as fibrin, producing a sticky clot that protects the wound. That clot is your body’s way of naturally bandaging the area and protecting the bare bone and nerves from air, foods you eat and bacteria.
It does more than just protect the clot. It is here inside the clot that healing cells known as fibroblasts and endothelial cells start to repair the tissue. The clot is then replaced by granulation tissue which becomes new gum or bone.
Normal Socket Healing What To Expect
A healing socket is supposed to progress in a regular point such a nature. Here’s what is going on day by day:
Day 1-2: A Blood Clot Forms On The Extraction Site This may come loose after a couple of days, and it’s not an issue if it does. This clot looks dark red, similar to a moist scab that is occupying the space in the hole where your tooth once sat. Some bleeding is expected for the first few days and you can expect swelling that will be at its height on day two or three.
Days 3-4: The clot is stable and could become darker, even close to brown or black in some cases. This change in color is a natural result of hemoglobin breaking down. Underneath, granulation tissue begins forming. Any pain that accompanied the removal should be subsiding at this time.
One Week: Those who can usually are weaned off or stop taking pain meds altogether. The clot formation is becoming established and the gum tissue is beginning to cover the empty socket. Risk of complications drops significantly.
Two Weeks: Tissue re-growth movement most had closed over the socket. There will be a faint indentation remaining, this is okay as long as there are no open wounds present.
One Month and More: In simple extractions, surface healing is nearly finished. Beneath it, bone regeneration carries on over the next few months.
What Is Dry Socket
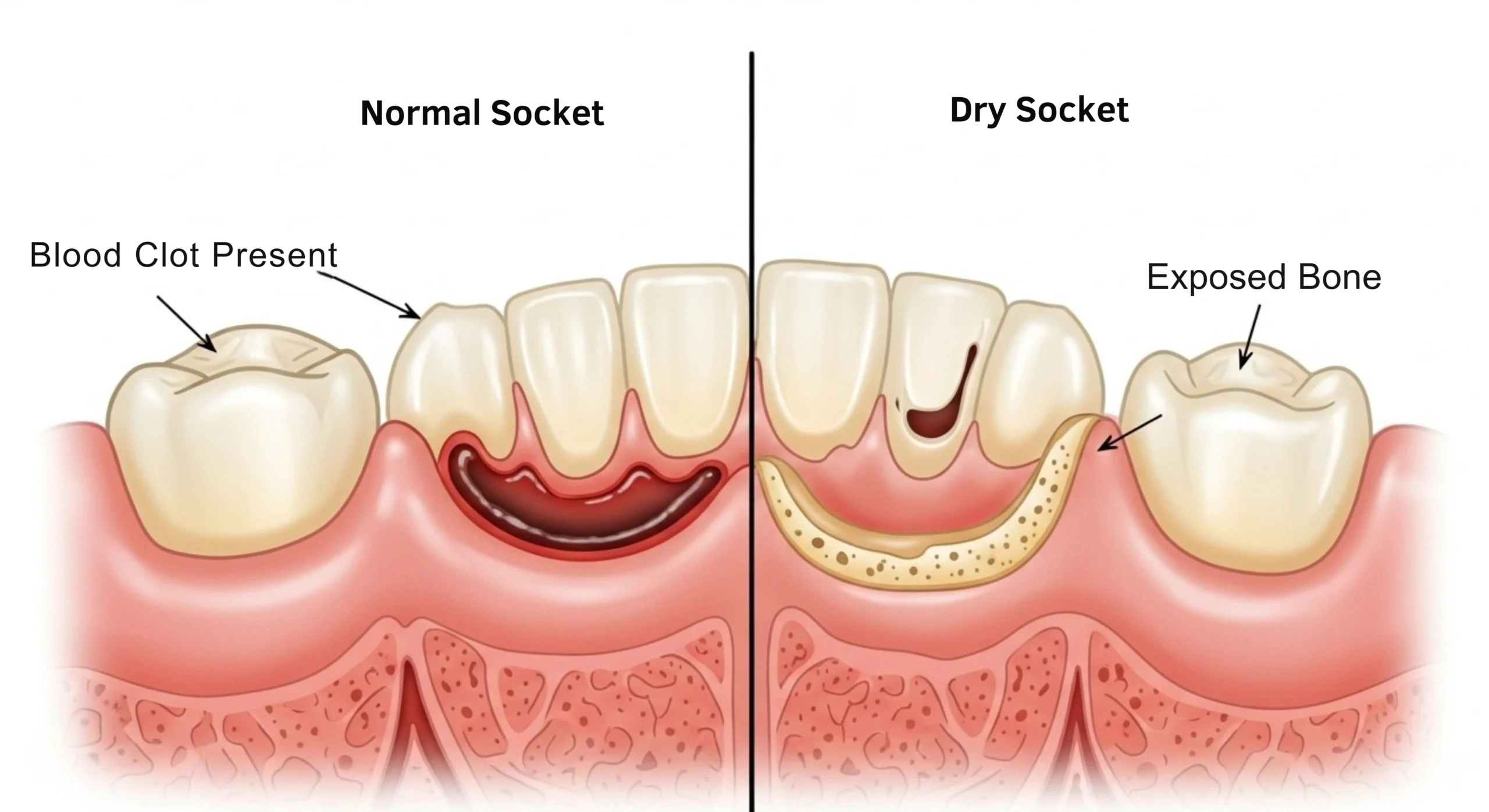
Dry socket, or alveolar osteitis in medical terms, happens when the protective blood clot doesn’t develop correctly or becomes dislodged before the wound has had time to heal. Without this clot, the bone and nerve endings are exposed to everything in your mouth.
The name “dry socket” is literal. The socket appears empty, with a whitish material at the base. That’s exposed bone there, and that is why this disorder hurts so bad.
Dry socket occurs 2-5 days following extraction when regular healing discomfort should be getting better.
How Common Is Dry Socket
The condition affects roughly 2-5% of all tooth extractions (Cleveland Clinic). However, the numbers change significantly based on the type of extraction.
Wisdom teeth, particularly impacted lower wisdom teeth, carry a much higher risk. Research indicates dry socket occurs in approximately 25-30% of impacted mandibular third molar extractions (NCBI Bookshelf – Alveolar Osteitis, StatPearls).
Dry Socket Vs. Normal Socket The Key Differences
Appearance:
Normal Socket: Contains a dark red or maroon blood clot that fills the extraction site. As healing progresses, you may see pink granulation tissue forming.
Dry Socket: Appears empty with visible whitish bone at the bottom. The protective clot is either absent entirely or only partially present. Food debris may accumulate in the empty space.
Pain Pattern:
Normal Socket: Pain is worst immediately after anesthesia wears off and improves steadily each day. Over-the-counter pain relievers usually provide adequate relief.
Dry Socket: Pain actually worsens 2-5 days after extraction, often becoming severe. The pain is typically described as throbbing and may radiate to your ear, eye, temple, or neck on the same side of your face. Standard pain medications often prove inadequate.
Other Symptoms:
Normal Socket: Mild swelling, slight tenderness, and minor bleeding that decreases over time.
Dry Socket: Bad breath, unpleasant taste in the mouth, possible low-grade fever, and visible bone in the socket. Notably, there is usually minimal external swelling or redness, which helps distinguish it from an infection.
Risk Factors for Dry Socket
Research has identified several factors that increase your chances of developing this painful condition.
Smoking:
Smoking represents one of the most significant risk factors. A systematic review published in Dentistry Journal in 2022 (Kuśnierek W, et al. “Smoking as a Risk Factor for Dry Socket: A Systematic Review“) found that tobacco smokers had more than three times the odds of developing dry socket compared to non-smokers. The same research found the incidence of dry socket was approximately 13.2% in smokers compared to 3.8% in non-smokers.
Smoking affects healing through multiple mechanisms. The sucking action can dislodge the clot, while chemicals in tobacco reduce blood flow to the socket and impair the clotting process.
Oral Contraceptives:
Women who take birth control pills are at higher risk. The research was published in the Journal of Oral and Maxillofacial Surgery (Catellani JE, et al. “Effect of oral contraceptive cycle on dry socket,” 1980) demonstrated an increased incidence of dry socket resulting from mandibular third molar extractions in the presence ORAL CONTRACEPTIVES of oral contraceptive use. The hazard seems to be linked with the impact of estrogen on fibrinolytic mechanisms in the circulation.
But also when you decide to pick. The latter study also found that risk could be reduced by scheduling extractions from days 23 to 28 of the tablet cycle, when estrogen effect is at its nadir.
Surgical Trauma:
Difficult extractions that require more manipulation increase dry socket risk. Impacted wisdom teeth, for example, often need bone removal and extended surgical time, both of which correlate with higher complication rates.
Poor Oral Hygiene:
Bacteria present in the mouth can interfere with clot formation and stability. Maintaining good oral hygiene before and after extraction helps reduce this risk.
Previous Dry Socket:
If you have developed dry socket after past extractions, you carry higher odds of experiencing it again.
Why Does Dry Socket Happen
The exact mechanism is not completely understood, but the fibrinolytic theory is widely accepted. This theory suggests that certain factors cause increased fibrinolysis, which is the process that breaks down fibrin in blood clots.
When fibrinolysis becomes excessive at the extraction site, the protective clot dissolves prematurely. Research published in the Journal of Oral Surgery (Nitzan DW. “On the genesis of dry socket,” 1983) established this connection between clot breakdown and dry socket development.
Physical disruption also plays a role. Sucking through straws, vigorous rinsing, or smoking can mechanically dislodge the fragile clot before it stabilizes.
Treatment Options
If you develop dry socket, your dentist will focus on relieving your pain while the socket heals naturally. The condition is self-limiting, meaning it will eventually resolve on its own, but treatment dramatically improves comfort.
Socket Irrigation:
Your dentist will gently flush out the socket using saline or an antiseptic solution. This removes food debris and bacteria while preparing the site for medicated dressings.
Medicated Dressings:
The most common treatment involves placing a medicated dressing directly into the socket. Alvogyl, containing eugenol (derived from cloves), iodoform, and butamben, is among the most frequently used dressings. A study published in the Journal of Oral and Maxillofacial Surgery (Faizel S, et al., 2015) found that Alvogyl provided effective initial pain relief compared to other dressings.
Eugenol has natural analgesic and antimicrobial properties, providing immediate relief while protecting the exposed bone. Zinc oxide eugenol dressings represent another common option.
Pain Management:
Over-the-counter medications like ibuprofen or acetaminophen help manage discomfort between dental visits. Your dentist may prescribe stronger pain medication if needed.
Follow-Up Care:
The dressing may need to be changed every few days until symptoms improve. Most patients require multiple visits during the healing process. With proper care, dry socket typically heals within 7-10 days.
How To Prevent Dry Socket
Taking precautions after extraction significantly reduces your risk.
Avoid Smoking:
The single most effective prevention measure for smokers is to abstain from tobacco. Avoid smoking for at least 48-72 hours after extraction, though longer is better. The sucking motion and chemicals in smoke both contribute to clot disruption.
Skip the Straw:
Drinking through a straw creates suction that can pull the clot from the socket. Drink directly from a cup for at least a week following extraction.
Be Gentle with Rinsing:
While keeping your mouth clean matters, vigorous swishing can dislodge the clot. After the first 24 hours, rinse gently with warm salt water by tilting your head rather than forcefully swishing.
Follow Post-Operative Instructions:
Your dentist provides specific guidelines for a reason. Following instructions about eating, drinking, activity level, and medication use supports proper healing.
Time Your Extraction:
If you take oral contraceptives, discuss timing with your dentist. Scheduling extraction during the low-estrogen phase of your cycle may reduce risk.
When To Contact Your Dentist
Reach out immediately if you experience:
- Severe pain that worsens 2-5 days after extraction
- Pain that radiates to your ear, eye, or temple
- An empty-looking socket without a visible blood clot
- Visible bone in the socket
- Bad breath or foul taste that was not present immediately after extraction
- Pain that does not respond to over-the-counter medication
Early intervention makes dry socket much more manageable. Most patients feel significant relief immediately after their dentist places a medicated dressing.
The Bottom Line
The difference between a normal healing socket and dry socket comes down to one thing: the blood clot. A healthy, intact clot means your body can heal as designed. A missing or dissolved clot leaves sensitive bone and nerves exposed, causing significant pain.
While dry socket is uncomfortable, it is also treatable. Understanding the warning signs helps you catch it early, and knowing the risk factors helps you take steps to prevent it in the first place. If you are scheduled for an extraction, follow your dentist’s aftercare instructions carefully. Those simple steps make a dramatic difference in your recovery experience.
References
Cochrane Database of Systematic Reviews. “Local interventions for the management of alveolar osteitis (dry socket)”.
Cleveland Clinic. “Dry Socket: Symptoms, Causes & Treatment”.
NCBI Bookshelf. “Alveolar Osteitis” (StatPearls, 2023).
Kuśnierek W, Brzezińska K, Nijakowski K, Surdacka A. “Smoking as a Risk Factor for Dry Socket: A Systematic Review.” Dentistry Journal. 2022;10(7):121.
Catellani JE, Harvey S, Erickson SH, Cherkin D. “Effect of oral contraceptive cycle on dry socket (localized alveolar osteitis).” J Am Dent Assoc. 1980;101(5):777-780.
Mamoun J. “Dry Socket Etiology, Diagnosis, and Clinical Treatment Techniques.” J Korean Assoc Oral Maxillofac Surg. 2018;44(2):52-58.
Akinbami BO, Godspower T. “Dry Socket: Incidence, Clinical Features, and Predisposing Factors.” Int J Dent. 2014.
Taberner-Vallverdú M, et al. “Efficacy of different methods used for dry socket management: A systematic review.” Med Oral Patol Oral Cir Bucal. 2015;20(5):e633-e639.
Faizel S, et al. “Comparision Between Neocone, Alvogyl and Zinc Oxide Eugenol Packing for the Treatment of Dry Socket.” J Maxillofac Oral Surg. 2015;14(2):312-317.
