Outie Vagina Are Normal Here What Every Woman Should Know
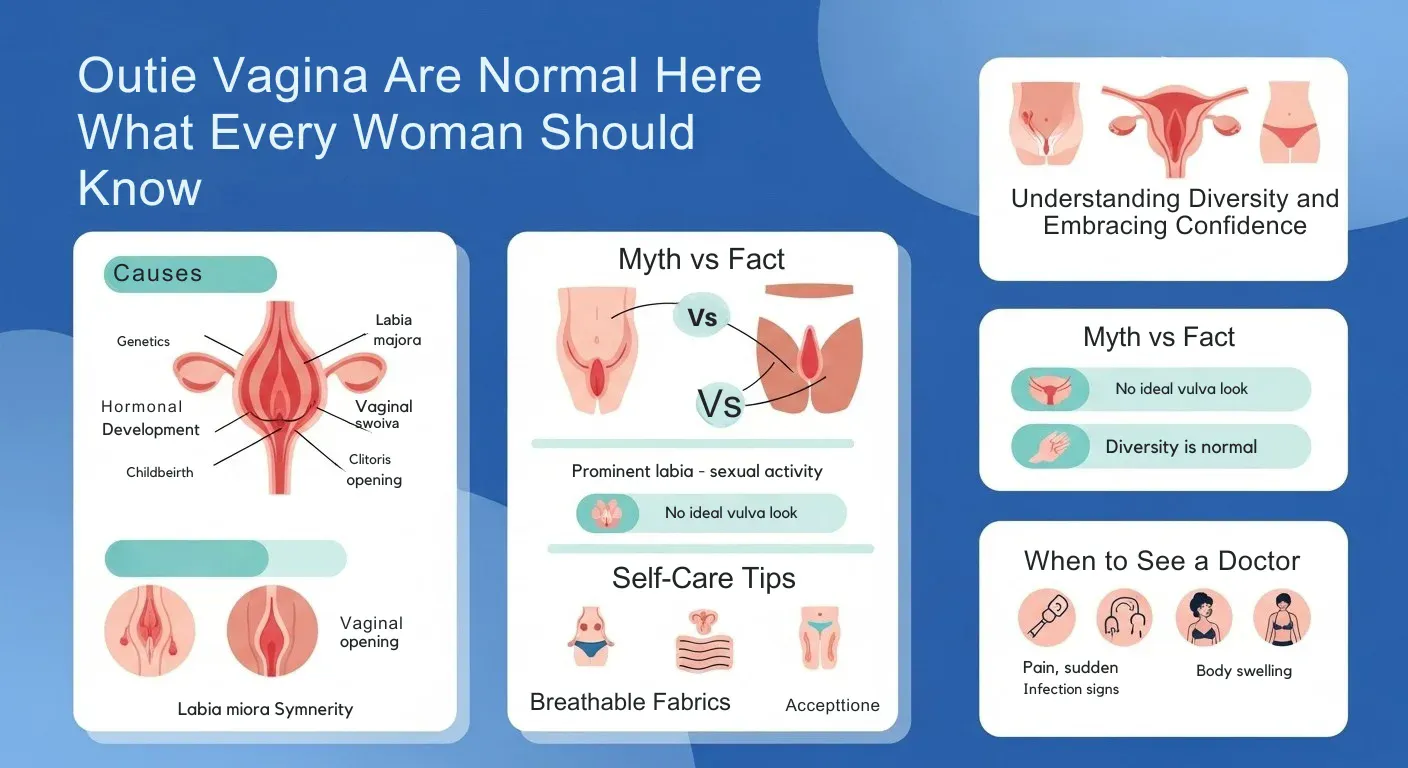
An “outie vagina” is an informal term for a common and normal variation in vulva appearance where the inner labia (labia minora) extend past the outer labia (labia majora). This appearance is determined by genetics and hormones, is not related to sexual activity or hygiene, and is found in up to half of all women. The key takeaway is that significant diversity in the size, shape, and color of the vulva is natural, and there is no single “normal” look. The article emphasizes embracing natural body variations for self confidence and encourages consulting a healthcare provider only if there is pain, persistent discomfort, or signs of infection.
| Anatomical Part | Common Term | Description |
|---|---|---|
| Labia Majora | Outer lips | The larger, fleshy outer folds of skin, often covered with pubic hair. |
| Labia Minora | Inner lips | The smaller, inner folds of skin that protect the vaginal and urethral openings. |
| Vulva | External genitals | Includes the labia, clitoris, and urethral/vaginal openings. |
| Vagina | Internal canal | The internal muscular passage leading from the vulva to the cervix. |
Understand Normal Vulvar Anatomy
‘Outtie vagina’ is an informal way of referring to a very common and completely normal variation in the appearance of the vulva, where the inner labia (the “lips”) are visible outside of or past the outer labia. This is an inherited sort of appearance, associated with hormones, and nothing to do with intercourse or hygiene, but present in up to half of all women.
Really, all that’s important here is there’s a huge variation in vulva size and shape, the same as penis or testicle size can vary and there is no one “normal” way they should look. The piece focuses on celebrating natural body diversity in the name of self-confidence “and then only if they hurt, itch a lot or they have signs of infection,” it reads.
What Causes Prominent Labia Minora
Genetics:
Your genetic inheritance is the primary factor determining labial size and appearance. Just as genes influence nose shape, ear size, and other physical characteristics, they also determine vulvar anatomy. If your biological mother or other female relatives have prominent labia minora, you’re more likely to have similar anatomy.
Hormonal Development:
“Outtie vagina” is slang discussing a very at least somewhat common and totally normal genital appearance variation, is which the inner labia (the “lips”) are what you see outside of or beyond the outer labia. This is the kind of looking a person inherits it’s to do with hormones, not sex or cleanliness but it happens in as many as one half of all females.
And truly, all that is worth noting here is there’s a vast range of vulva sizes and shapes, the same as what penis or testicle size can look like just like no one “normal” way these bits should appear. The story emphasizes that we should embrace our God-given natural diversity in a celebration of self-confidence “and only then if they are painful, itch excessively or have signs of infection,” it reminds us.
Age-Related Changes:
As women age, the labia majora may lose subcutaneous fat and elasticity. This natural aging process can make the labia minora appear more prominent, even if they haven’t actually changed in size. The loss of estrogen during menopause can also affect vulvar tissues, though changes vary significantly among individuals.
Childbirth:
Vaginal delivery involves stretching of the vulvar and vaginal tissues. While most changes are temporary, some women notice their labia appear different after giving birth. This is a normal part of postpartum body changes and doesn’t indicate any problem.
Other Factors:
Physical activities like cycling, horseback riding, or certain sports don’t permanently change labial size, though they may cause temporary swelling or irritation. Weight fluctuations can affect the fatty tissue in the labia majora but don’t significantly impact the labia minora, which contain less fat tissue.
Debunking Harmful Myths
Prominent Labia Are Caused by Sexual Activity:
This is completely false and rooted in harmful, sexist misconceptions about female sexuality. Sexual activity, masturbation, and the use of tampons or menstrual cups do not stretch or permanently change the labia. The vulva and vagina are designed to accommodate penetration and return to their baseline state.
This myth has been used historically to shame women and attempt to judge their sexual history based on genital appearance—something that is anatomically impossible and ethically reprehensible.
Myth 2: There’s an “Ideal” Vaginal Appearance
The cosmetic surgery industry, pornography, and digitally altered images have created false standards of what vulvas “should” look like. These images often show only one type of vulvar appearance—typically with minimal or hidden labia minora—which represents just a small portion of the natural spectrum.
Medical research and anatomical studies have documented that vulvar diversity is the norm, not the exception. No single appearance is more “normal” or “correct” than another.
Prominent Labia Indicate Poor Hygiene:
Labial size has absolutely no relationship to hygiene. The vulva is self-cleaning, and proper genital care is the same regardless of labial anatomy. This myth causes unnecessary shame and can actually lead to harmful practices like douching or using harsh soaps, which disrupt the natural vaginal pH and can cause infections.
It Will Interfere with Sexual Function:
For the vast majority of women, prominent labia minora don’t interfere with sexual activity, pleasure, or function. The labia minora are rich in nerve endings and contribute to sexual sensation. Many women find that labial stimulation enhances pleasure.
Only in rare cases where the labia are extremely large and cause pulling or discomfort during intercourse might there be functional concerns worth discussing with a healthcare provider.
Prominent Labia Are Abnormal or a Medical Condition:
Unless labial size causes functional problems with daily activities, exercise, or intimacy, prominent labia minora are not a medical condition requiring treatment. They’re simply a normal anatomical variation, like having larger breasts or a longer nose.
When to Consult a Healthcare Provider
While prominent labia are typically normal, certain symptoms warrant medical evaluation:
Sudden Changes:
If your labia suddenly increase in size, especially if accompanied by pain, redness, warmth, or discharge, this could indicate infection or another medical issue requiring evaluation.
Persistent Pain or Discomfort:
If you experience ongoing pain during walking, sitting, exercise, or sexual activity that interferes with your quality of life, consult a gynecologist. While most prominent labia don’t cause discomfort, true labial hypertrophy (medically significant enlargement) can occasionally cause functional problems.
Signs of Infection:
Seek medical attention if you notice:
- Unusual discharge with a foul odor
- Severe itching or burning
- Visible sores, blisters, or lesions
- Significant swelling that develops rapidly
- Fever or feeling unwell
Lumps or Cysts:
Bartholin’s gland cysts can cause painful, one-sided labial swelling. These fluid-filled cysts occur when the glands near the vaginal opening become blocked. While they can sometimes resolve on their own, infected cysts (abscesses) require medical treatment.
Psychological Distress:
If concerns about your genital appearance are causing significant anxiety, depression, or avoidance of intimacy, speaking with a mental health professional can be helpful. Body image concerns about the genitals are common but shouldn’t interfere with your quality of life or self-esteem.
Medical Conditions That May Affect the Labia
While most labial prominence is simply normal variation, occasionally it may be associated with:
Labial Hypertrophy:
This medical term describes labia minora that are enlarged enough to cause functional problems. There’s no consensus on the exact measurement that defines hypertrophy, but functional symptoms matter more than size alone.
Lymphedema:
Rarely, chronic lymphatic obstruction can cause labial swelling. This is typically accompanied by swelling in other areas and requires medical evaluation.
Hormonal Disorders:
Conditions affecting androgen (male hormone) levels can sometimes cause labial changes, though this is uncommon and would typically be accompanied by other symptoms like excessive hair growth or menstrual irregularities.
Vulvar Dermatologic Conditions:
Skin conditions like lichen sclerosus, lichen planus, or chronic inflammation can affect vulvar tissues and appearance. These conditions require proper diagnosis and treatment by a healthcare provider.
Treatment and Management Options
Conservative Approaches:
For most women, no treatment is necessary. If you experience minor irritation or chafing:
Clothing choices: Wear breathable cotton underwear and avoid tight pants or leggings that cause friction. Seamless underwear can reduce irritation.
Activity modifications: If you experience discomfort during cycling or certain exercises, padded shorts or adjusting your positioning may help.
Barrier protection: Use petroleum jelly or other barrier creams on the labia before extended exercise to prevent chafing.
Gentle hygiene: Cleanse the vulvar area with warm water or a gentle, fragrance-free cleanser. Avoid douches, scented products, and harsh soaps.
Proper wiping: Always wipe from front to back after using the bathroom to prevent bacterial transfer from the anus.
Surgical Options: Labiaplasty:
Labiaplasty is a surgical procedure to reduce the size of the labia minora. This surgery should only be considered when there are genuine functional problems not for cosmetic concerns alone.
Important considerations about labiaplasty:
Risks: Like any surgery, labiaplasty carries risks including infection, bleeding, scarring, asymmetry, loss of sensation, chronic pain, and dissatisfaction with aesthetic results. Nerve damage can affect sexual sensation.
Effectiveness: While surgery can reduce labial size, it cannot guarantee specific aesthetic outcomes, and revision surgery is sometimes needed.
Age considerations: Medical organizations strongly advise against labiaplasty for minors except in cases of congenital abnormalities causing functional problems. The genitals continue developing through late adolescence, and performing surgery during development can lead to poor outcomes.
Psychological factors: Research suggests that many women seeking labiaplasty don’t have labial measurements outside the normal range but rather have concerns driven by unrealistic expectations about genital appearance. Psychological counseling may be more appropriate than surgery for appearance-based concerns.
Insurance coverage: Most insurance plans don’t cover labiaplasty when performed for cosmetic reasons, as it’s considered elective surgery.
The Role of Media and Pornography
The internet age has exposed people to countless images of genitals, but these images are often highly curated, edited, and unrepresentative of natural diversity. Pornography typically features performers with one specific type of vulvar appearance, and these images are frequently digitally altered.
This narrow representation has contributed to increased anxiety about genital appearance, particularly among younger women. Some research has linked increased pornography exposure to body image concerns and requests for cosmetic genital surgery.
Educational resources showing the true diversity of vulvar anatomy can help counter these unrealistic standards and promote body acceptance.
Talking to Your Healthcare Provider
If you have concerns about your labial appearance or function, a gynecologist or primary care provider can provide reassurance and guidance. During a pelvic exam, they can:
- Confirm that your anatomy is within the normal range
- Check for any underlying medical conditions
- Discuss whether your symptoms indicate functional problems
- Provide advice on managing minor discomfort
- Refer you to appropriate specialists if needed
Remember that healthcare providers see enormous anatomical diversity and won’t judge your appearance. If you feel uncomfortable with your provider’s response to your concerns, seeking a second opinion is always appropriate.
Supporting Body Positivity and Acceptance
Understanding that genital diversity is normal and natural is crucial for mental health and self-acceptance. The growing body positivity movement has helped many women develop healthier relationships with their bodies, including their genitals.
Some helpful approaches include:
Education: Learning about normal anatomical variation can reduce anxiety and increase acceptance.
Rejecting harmful comparisons: Recognizing that media images don’t represent reality helps counter unrealistic standards.
Focusing on function: Your genitals’ ability to provide pleasure and function normally matters far more than appearance.
Seeking support: If body image concerns are affecting your life, therapy can help address underlying anxiety or self-esteem issues.
Open communication: Talking with trusted partners about insecurities can help you feel more comfortable and accepted.
The Bottom Line
An “outie vagina” or more accurately, prominent labia minora is a completely normal anatomical variation experienced by millions of women. This appearance is primarily determined by genetics and doesn’t indicate anything about your sexual history, hygiene, or health. Unless you’re experiencing genuine functional problems like persistent pain during daily activities or intercourse, your anatomy doesn’t require any treatment or intervention.
The vast majority of labial size variations are simply part of human diversity, like having different eye colors or heights. If you’re feeling anxious about your genital appearance, remember that medical research has documented enormous natural variation in vulvar anatomy. What you see in curated media images doesn’t represent the full spectrum of normal human bodies. Focus on health, function, and self-acceptance rather than achieving an arbitrary aesthetic standard. Your body is normal, and you deserve to feel comfortable and confident in your own skin.
References:
- American College of Obstetricians and Gynecologists – Committee Opinion on Vaginal “Rejuvenation” and Cosmetic Vaginal Procedures.
- Royal Australian College of General Practitioners – Female Genital Cosmetic Surgery Guidelines.
- British Society for Paediatric and Adolescent Gynaecology – Statement on Labiaplasty in Adolescents.
- NHS UK – Labiaplasty Information and Guidelines.
- Mayo Clinic – Vulvar Anatomy and Health Information.
- Cleveland Clinic – Women’s Health and Gynecology Resources.
