Cardiac Arrest: Signs, Symptoms, Treatment

You are with someone who suddenly falls to the floor, doesn’t respond, doesn’t breathe, and you feel no pulse. It’s terrifying, This kind of scenario is not only dramatic it’s cardiac arrest. It’s one of those medical emergencies where every second counts. You’ll learn what cardiac arrest is, how it’s different from a heart attack, what signs and symptoms to watch for, how treatment works, and most importantly, what you (yes, you!) can do to help.
What Is Cardiac Arrest
Cardiac arrest happens when the heart suddenly stops pumping blood. This can be due to a problem with the heart’s electrical system. Without blood moving, oxygen doesn’t get to your brain or organs. Without quick action, irreversible damage or death follows.
How Is Cardiac Arrest Different from a Heart Attack
These terms often get mixed up, but they’re not the same:
- Heart attack usually means a blockage in a blood vessel supplying the heart muscle. The heart still may beat, but it’s starved of oxygen.
- Cardiac arrest means the heart stops beating effectively no circulation. It can happen during or after a heart attack, but also without one.
Signs and Symptoms: What to Watch For
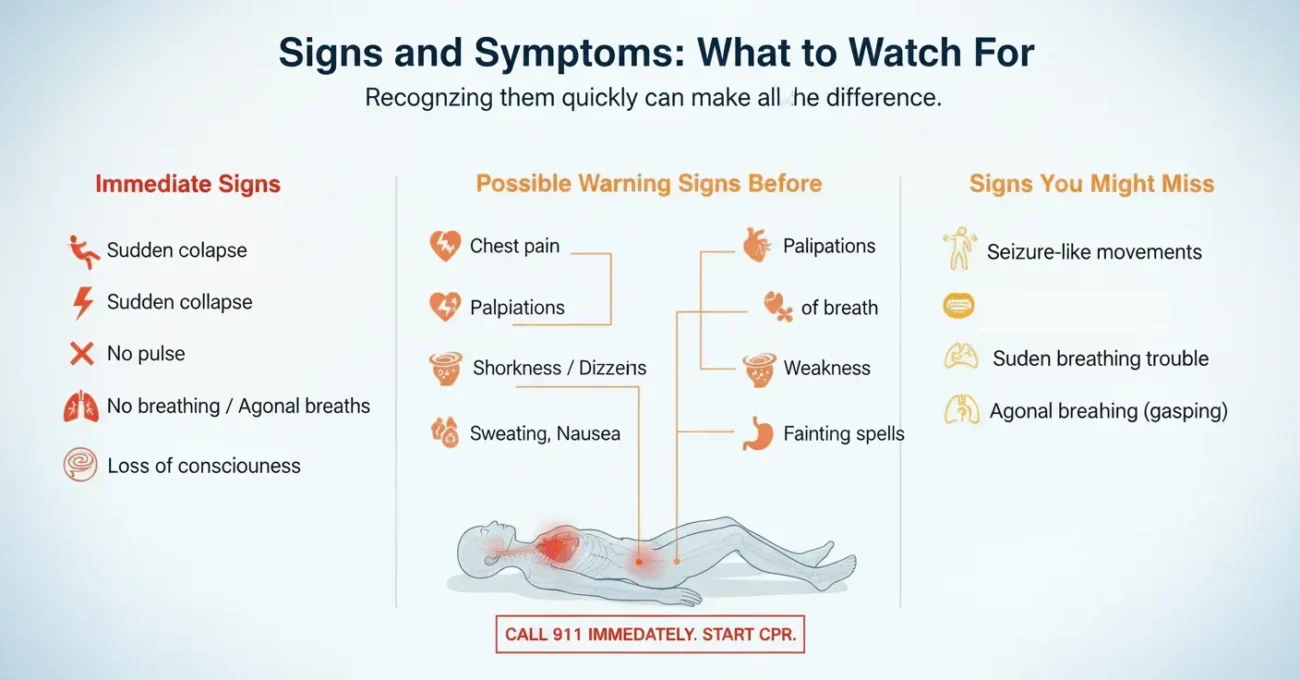
Often cardiac arrest comes without warning. But sometimes, there are clues. Recognizing them quickly can make all the difference.
Immediate signs
These are the red-flags when cardiac arrest is happening:
- Sudden collapse (falls down, loses consciousness) with no response.
- No pulse.
- No breathing or very abnormal breathing (gasping or “agonal” breaths).
- Loss of consciousness.
Possible warning signs before the event
Sometimes, though not always, people notice symptoms before things go terribly wrong:
- Chest discomfort or pain (but not always).
- Palpitations: heart racing, fluttering, or beating oddly.
- Shortness of breath even at rest or with mild activity.
- Feeling very weak, dizzy, or lightheaded.
- Fainting, or near-fainting spells.
- Sweating, nausea even sometimes vomiting.
Signs you might miss
- Seizure-like movements (sometimes cardiac arrest is mistaken for seizure).
- Sudden breathing trouble that isn’t typical asthma or cough.
- Agonal breathing: gasps, not real breaths. Many bystanders don’t recognize this.
What Causes Cardiac Arrest
Knowing what can lead to cardiac arrest helps in prevention and awareness.
Electrical system failures
Problems with the heart’s rhythm (arrhythmias). For instance, ventricular fibrillation (the ventricles quiver instead of pumping properly). Long QT syndrome, Brugada syndrome, or other inherited rhythm issues.
Structural heart problems
- Coronary artery disease (blockages in hearts arteries).
- Cardiomyopathy (heart muscle becomes thick, weak, or stiff).
- Heart valve disease.
- Congenital heart defects (birth defects).
Treatment
When cardiac arrest happens, treatment has to be fast. The quicker the help, the better the chance of survival.
Recognize and call for help
If you see someone collapse and they’re not breathing normally, shout for help. Call emergency services immediately. Don’t wait.
CPR (Cardiopulmonary Resuscitation)
Start chest compressions right away. Push hard and fast in the center of the chest. If you’re trained, you add rescue breaths. If not, do hands-only CPR (just compressions). The aim is to keep blood moving until professionals arrive. Every minute without CPR reduces survival chances drastically.
Use an AED
If there’s an AED nearby, use it. AEDs are made for laypeople: they often give voice prompts. They can deliver a shock to reset the heart’s rhythm. Using one early (within minutes) improves survival a lot.
Advanced medical care
Once emergency medical services arrive, they might:
- Give medicines to support heart rhythm and blood pressure.
- Use more advanced defibrillation.
- Intubate (provide airway support) if needed.
- Perform tests (EKG, blood tests, imaging) to find underlying cause.
- Possibly implant devices like ICDs (implantable cardioverter-defibrillators) for people known to be at high risk.
Prevention You Can Take Ahead of Time
It’s always better to prevent than to treat. Here are ways to reduce your chances, and help others be prepared.
- Keep up with health checkups: heart health, cholesterol, blood pressure.
- Get screened for heart rhythm disorders if family history or symptoms.
- Stay active; exercise regularly but safely.
- Eat a heart-friendly diet.
- Avoid tobacco and limit alcohol.
- Stay alert to symptoms, don’t ignore weird palpitations, fainting, chest discomfort.
- If you’re in a public place, know where AEDs are. Encourage them to be installed in public spots.
- Learn CPR even hands-only CPR is extremely useful. Encourage your family, friends, workplace to train.
FAQs
Q: Can someone survive a cardiac arrest without treatment?
A: Very rarely, and only if help comes immediately. Without CPR or defibrillation, brain damage starts within minutes.
Q: How quickly must CPR start?
A: Immediately. Ideally within the first minute after collapse. Every minute delay reduces survival rates significantly.
Q: Is CPR safe for the person doing it?
A: Yes. Doing CPR on someone who’s unconscious and not breathing won’t harm them; delaying CPR definitely harms. For the rescuer, minor rib fractures are possible; but saving life outweighs those risks.
Q: Is it always obvious when someone is having cardiac arrest?
A: No. Sometimes there are warning signs; sometimes there are none. And breathing may look odd (gasping) but isn’t effective breathing. Recognizing that no breathing + no responsiveness = emergency can save lives.
Q: What is the role of an ICD?
A: An ICD is a small device implanted in the chest that monitors heart rhythm. If it detects a dangerous arrhythmia, it delivers a shock to restore normal rhythm. Useful for people who are at high risk.
Conclusion
Cardiac arrest is scary, but unlike many emergencies, your actions do matter. Recognizing it quickly, calling for help, starting CPR, using an AED if available these can rescue someone from the brink. By knowing the signs and treatment, by spreading this knowledge, by pushing for CPR training and AED access in your community you become part of the lifeline. You might never need this, but if you do, you’ll be ready.
